What are the top LPN interview questions and how should you answer them?
LPN interviews test more than clinical skill—they assess your judgment, ethics, teamwork, and communication. Be ready for scope-of-practice, prioritization, and behavioral questions. Use structured, evidence-based answers that demonstrate calm decision-making, empathy, and professionalism. The best answers show both competence and emotional intelligence under pressure.
Landing your next LPN role takes more than listing clinical skills.
Employers want nurses who demonstrate clear role understanding, sound judgment, and composure under pressure - generic answers won’t cut it.
And with the U.S. Bureau of Labor Statistics projecting a steady 3% growth in LPN jobs from 2024-2034, competition for top positions remains strong, especially across nursing and residential care facilities.
That’s why thoughtful interview preparation is key - it’s your chance to show not just what you know, but how you think, act, and communicate under real-world conditions.
This guide breaks down the questions hiring managers really ask, why they ask them, and how to deliver answers that set you apart.
1. The Scope Question
Question: "Describe a time an RN's care plan for a patient seemed off. What did you do?"
Why they ask: This is a test of your professionalism and, most importantly, your understanding of scope of practice. A common mistake LPNs make in interviews is confusing their role with an RN's. They want to see that you know your job is to observe, gather data, and report - not to make a final "medical interpretation" or unilaterally change a plan.
What not to say: "I told the RN they were wrong and just did what I thought was right. I know my patients." This shows a dangerous disregard for the nursing chain of command.
A Standout Answer:
"I was caring for a patient with stable vitals who was suddenly prescribed a high-dose diuretic in their chart by the RN. I knew this patient's baseline from my morning assessment, and this new order seemed unusual. My first step was to re-take the patient's vitals, paying close attention to their blood pressure and any signs of edema. I then approached the RN privately, stated my objective findings 'Mr. Smith's blood pressure is 110/60, and his chart notes are stable', and respectfully asked for clarification on the new order. The RN had mistaken the patient for another. By presenting my data calmly and asking questions, we corrected the potential error before it reached the patient. My role is to be the RN's eyes and ears, and that's what I did."
2. The Prioritization Question
Question: "It's 10 a.m. You have a patient complaining of 8/10 pain, another patient needs a complex wound dressing change, and a third patient's family is at the desk complaining loudly. What do you do first?"
Why they ask: This isn't just about time management; it's a test of your clinical judgment. They need to know you can distinguish between a critical clinical need and a loud logistical need.
What not to say: "I'd go to the complaining family first to calm them down." This shows you react to the "loudest" problem, not the most medically urgent one.
A Standout Answer:
"My immediate priority is the patient in 8/10 pain, as uncontrolled pain is a critical clinical sign that needs assessment. I would first perform a quick, 60-second assessment on that patient to ensure their vitals are stable and the pain isn't a symptom of a new, life-threatening event, like a cardiac issue. I would tell them I am getting their medication immediately.On my way to the med room, I would make eye contact with the family at the desk, tell them 'I see you and will be with you in just one moment,' and then ask the unit secretary to offer them a seat in a private room.After administering the pain medication, I would address the family's concerns. Finally, I would proceed with the complex wound dressing change, which is an important task but not as time-sensitive as acute pain."
3. The Behavioral Question
Question: "Tell me about a time you had a difficult time building rapport with a patient."
Why they ask: They know not every patient is easy. They want to see your communication skills, patience, and empathy in action. Research confirms a "statistically significant positive correlation" between nurse-patient communication and patient satisfaction. In fact, one study found that weak communication directly led to poor patient satisfaction scores.
What not to say: "Some patients are just impossible, and you can't waste time on them. I just do my tasks and leave."
A Standout Answer:
"I was caring for a resident who was consistently short with me and would refuse care. I made a point to read their chart and saw they were a retired history professor. The next day, instead of starting with my tasks, I mentioned a history documentary I had seen. Their eyes lit up. We talked for just five minutes about it, and the entire dynamic changed. I learned they felt invisible and that no one talked to them, only at them. By connecting with them as a person first, I built the trust needed to provide care. It taught me that rapport isn't just 'nice'—it's a core part of the care plan."
4. The Ethical Question
Question: "A patient with dementia is refusing a medication, but you know they need it. How do you handle this?"
Why they ask: This question pits two core nursing values against each other: patient autonomy and a nurse's duty to care (beneficence). They are looking for your understanding of consent, your patience, and your knowledge of de-escalation techniques, especially for geriatric patients.
What not to say: "I'd crush it up in their applesauce. They need it, and they won't remember anyway." This is a major ethical violation and a fireable offense.
A Standout Answer:
"First, I would never force the medication. Even with a dementia diagnosis, the patient has a right to refuse. I would put the medication aside and try to identify the 'why' behind the refusal. Are they in pain? Is the pill hard to swallow? Are they frightened?I would leave the room for a few minutes and come back, re-introducing myself and the medication in a calm, friendly way. If they still refused, I would try again in 20-30 minutes. If the refusal continues, I would document it, note my re-attempts and the patient's response, and inform the RN and the prescribing provider. My final step is to document the refusal and my interventions, ensuring the entire care team is aware."
Also Read: How to build a career in the healthcare industry?
5. The "In-Demand" Skill Question
Question: "What's your experience with [Wound Care/IV Therapy/EHR Charting]?"
Why they ask: Facilities need LPNs with specific, high-value skills. Hiring managers are looking for candidates who have invested in their careers. Holding certifications in areas like Wound Care (CWCA), IV Therapy, or Long-Term Care (CLTC) makes you a much more valuable asset. Proficiency in Electronic Health Records (EHR) is no longer optional; it's a core competency.
What not to say: "I'm not certified in that, but I'm a fast learner."
A Standout Answer (if you have the skill):
"I'm actually IV therapy certified. In my last role, I was responsible for initiating and monitoring peripheral IVs for 20 residents. I'm also proficient in managing and documenting complex wound dressing changes and have experience with wound vacs. In terms of EHRs, I've used PointClickCare for the last three years, particularly for e-MAR and tracking patient ADLs."
A Standout Answer (if you don't):
"While I don't currently hold a wound care certification, it's my next professional goal. I've actively managed Stage 1 and Stage 2 pressure ulcers, including documentation and reporting. I am, however, highly proficient in the [X] EHR system and am known for my detailed and accurate nursing charting."
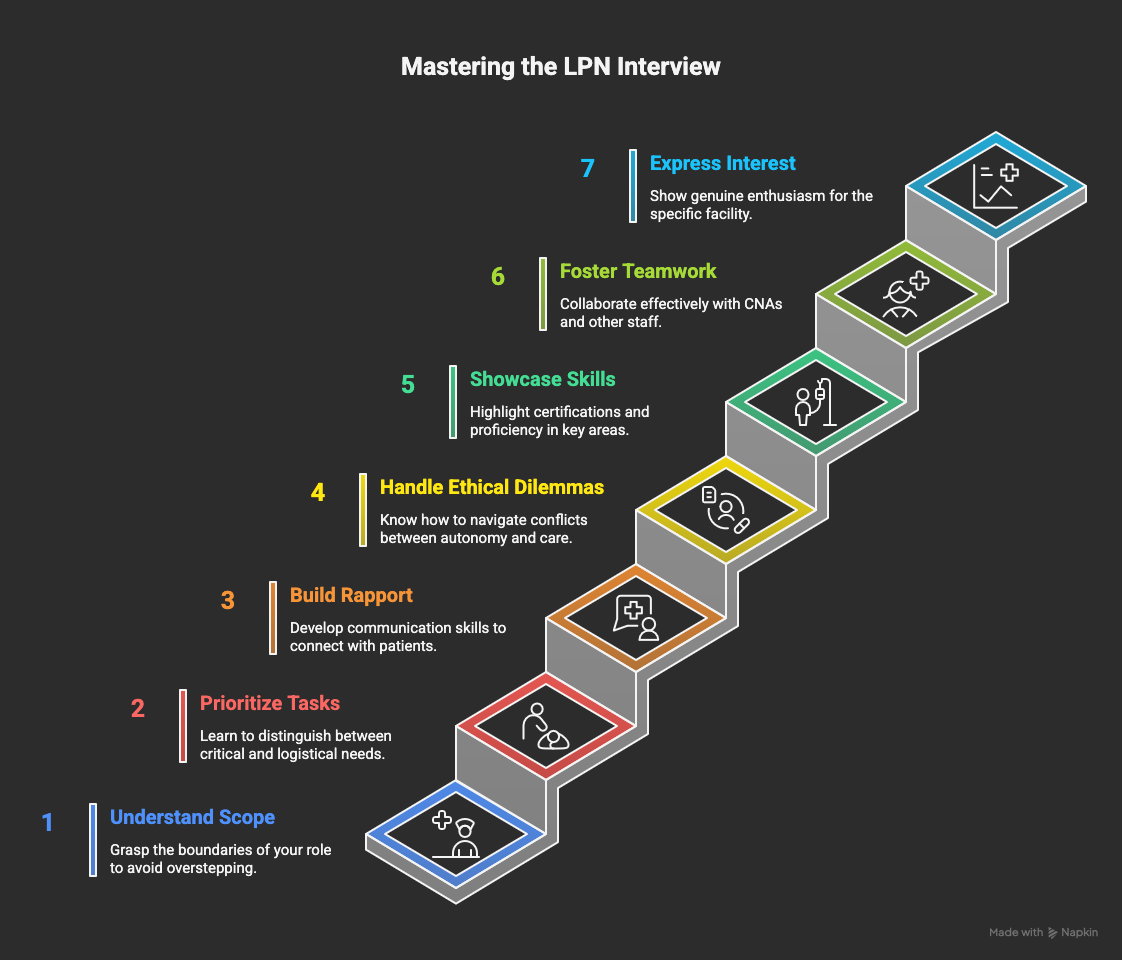
6. The Teamwork Question
Question: "Describe your relationship with the CNAs on your previous unit."
Why they ask: LPNs are the clinical leaders and supervisors for CNAs. A poor relationship with CNAs means care breaks down. Studies on nursing home care quality show that outcomes are better when the LPN's role is clearly defined and they work well with the entire team. They want to know you are a leader and a partner, not a dictator.
What not to say: "I just told them what to do. It's not my job to be their friend."
A Standout Answer:
"I view the CNAs as my essential partners. I make it a rule to never ask a CNA to do something I wouldn't do myself. I always start my shift by checking in with them, asking what they observed with residents. They're the ones providing the most hands-on care and are often the first to spot a subtle change. I treat them with respect, provide clear instructions, and always have their back. When they feel respected, the entire team functions better, and patient care improves."
7. The "Why Us" Question
Question: "Why are you interested in our long-term care facility specifically?"
Why they ask: They want to know you've done your research and aren't just one of 100 job applications. They want to see a genuine interest in their specific patient population, such as geriatrics, rehab, or palliative care.
What not to say: "I need a job, and you're hiring. The commute is good."
A Standout Answer:
"I've been following your facility since you received the 5-star quality rating from CMS. I was particularly impressed by your low patient re-hospitalization rates, which tells me you have strong clinical protocols. My passion is in geriatric and hospice and palliative care, and I know your facility has a dedicated palliative-certified nurse. I want to work in an environment that prioritizes that level of specialized, compassionate care, and I'm eager to contribute my skills to your team."
Wrapping Up
Interviewing for an LPN role isn’t just about answering questions correctly; it’s about showing clinical judgment, emotional intelligence, and confidence in your scope of practice.
When you prepare with intention, you walk in ready to communicate clearly, think critically, and demonstrate the kind of professionalism hiring managers look for.
And if you’re looking to sharpen your resume, strengthen your interview prep, or present your clinical experience more effectively on LinkedIn, Hiration can support you with tools designed to help healthcare professionals stand out.
With the right preparation, you’re not just hoping for the job, you’re ready for it.
LPN Interview Prep — FAQ
What’s the best way to handle a “scope of practice” question?
Emphasize teamwork and chain of command. Show that you know your limits—LPNs observe, record, and report findings, not diagnose or alter care plans independently.
How do I answer prioritization scenarios?
Always prioritize clinical urgency over convenience or noise. Start with the patient in potential distress, then manage non-urgent or administrative concerns calmly and efficiently.
What if I’m asked about a difficult patient?
Use a real example that highlights empathy, patience, and active listening. Show how you adapted communication to build rapport and improve cooperation.
How do I approach ethical questions about patient refusal?
Show respect for autonomy. Explain that you would pause, assess underlying causes, attempt again calmly, and document all refusals while notifying the RN or provider.
What if I lack certain certifications or clinical skills?
Don’t apologize. Express your plan to earn them soon and highlight related experience. Focus on what you can do well, like accurate charting or wound monitoring.
How should I describe teamwork with CNAs?
Frame it as partnership and respect. Show that you listen to their input, communicate clearly, and lead by example to ensure consistent patient care.
What’s the right way to answer “Why our facility?”
Show genuine research. Reference the facility’s ratings, programs, or care model. Connect these to your personal passion areas like geriatrics, rehab, or palliative care.
Can Hiration help with LPN interview preparation?
Yes. Hiration helps healthcare professionals craft resumes, prepare for interviews, and polish LinkedIn profiles—so your skills and professionalism stand out clearly to employers.



